As a physician, healthcare executive, and innovator, I’ve been closely following the rapid advancements in artificial intelligence and their potential impact on healthcare. While the promise of AI in revolutionizing healthcare is immense, a recent analysis by Epoch AI on the scalability of AI training gives us pause to consider whether these promises can be fully realized by 2030. Let’s explore the potential roadblocks that could prevent AI from reaching the “promised land” in healthcare by the end of this decade.
The Current Trajectory of AI in Healthcare.
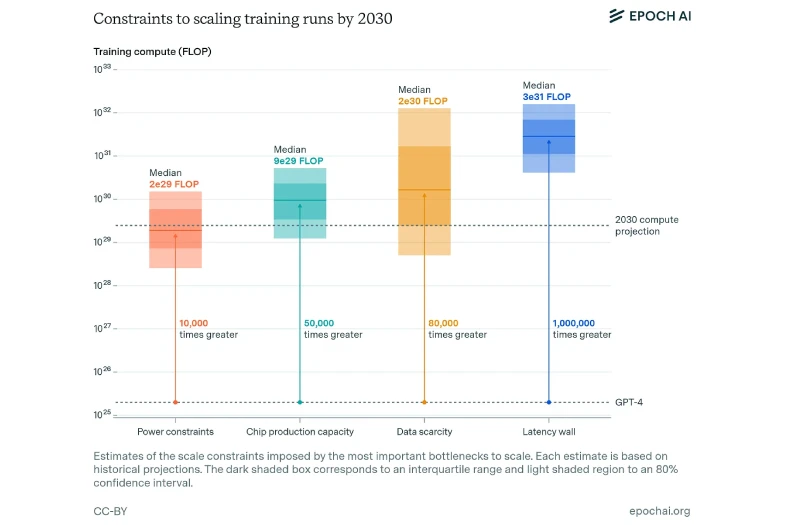
The healthcare sector has seen remarkable progress in AI applications, from diagnostic imaging to drug discovery. This growth in AI capabilities is largely driven by increases in computational resources, with AI training compute expanding at a staggering rate of approximately 4x per year. If this trend were to continue unabated, by 2030 we might expect AI models in healthcare that far exceed current state-of-the-art systems. This could theoretically translate to AI systems capable of complex medical reasoning, personalized treatment planning, and even assisting in intricate surgical procedures. However, the Epoch AI analysis identifies four critical factors that could constrain AI scaling: power availability, chip manufacturing capacity, data scarcity, and computational latency. Let’s consider how these factors might impact healthcare AI specifically:
- Power Availability:
While the analysis suggests that AI training facilities capable of 2 to 5 gigawatts of power demand may be feasible by 2030, the healthcare sector may face unique challenges. Hospitals and healthcare facilities, already under pressure to reduce their carbon footprint, may struggle to justify the enormous energy consumption required for large-scale AI training. - Chip Manufacturing Capacity:
The projected chip production capacity could support massive AI models, but healthcare-specific AI may not be the priority for chip manufacturers. With competition from other sectors like finance and autonomous vehicles, healthcare AI developers might face supply constraints and higher costs. - Data Scarcity:
Healthcare data is abundant but fraught with privacy concerns and regulatory restrictions. While synthetic data generation offers some promise, it may not fully replicate the complexity and nuance of real-world healthcare data. This could limit the scale and effectiveness of healthcare AI models. - Computational Latency:
In critical care scenarios, even milliseconds of delay can have life-or-death consequences. The latency issues identified in the Epoch AI analysis could prove particularly problematic for real-time healthcare applications, potentially limiting AI’s role in urgent clinical decision-making.
Additional Healthcare-Specific Challenges.
Beyond these general constraints, healthcare faces unique hurdles in AI adoption:
- Regulatory Hurdles:
The healthcare industry is heavily regulated, and AI systems will need to clear stringent approval processes. This could significantly slow the deployment of advanced AI models in clinical settings. - Integration with Legacy Systems:
Many healthcare providers still rely on outdated IT infrastructure. Integrating cutting-edge AI systems with these legacy systems could prove technically challenging and prohibitively expensive. - Clinician Adoption:
There’s often resistance to new technologies in healthcare settings. Convincing clinicians to trust and adopt AI systems, especially as they become more complex, could be a significant barrier. - Ethical Concerns:
As AI models become more powerful, ethical questions about their use in healthcare decision-making will intensify. Resolving these ethical dilemmas could slow AI adoption. - Health Equity:
There’s a risk that advanced AI systems could exacerbate existing health disparities if they’re not accessible to all healthcare providers and patients.
Mitigating Challenges in AI Scaling for Healthcare
While the potential of AI in healthcare is immense, the challenges identified in the Epoch AI analysis suggest that we may not reach the “promised land” of AI capabilities as quickly as some predict. However, there are several strategies healthcare leaders can employ to mitigate these challenges and continue making progress:
- Addressing Power Constraints:
- Invest in energy-efficient AI hardware and algorithms
- Explore distributed computing models that spread computational load across multiple facilities
- Advocate for policies that support renewable energy development for healthcare AI applications
- Navigating Chip Manufacturing Limitations:
- Form strategic partnerships with chip manufacturers to ensure access to cutting-edge hardware
- Invest in AI model optimization techniques that maximize performance on existing hardware
- Explore cloud-based AI solutions that can leverage shared computing resources
- Overcoming Data Scarcity:
- Invest in synthetic data generation techniques to augment existing datasets
- Develop federated learning approaches that allow AI models to learn from distributed datasets without compromising privacy
- Establish data sharing partnerships with other healthcare organizations to create larger, more diverse datasets
- Managing Computational Latency:
- Prioritize AI applications that can tolerate some delay, focusing on non-real-time tasks first
- Invest in edge computing solutions for latency-sensitive applications
- Develop hybrid models that combine lightweight, low-latency models for immediate decisions with more complex models for deeper analysis
- Focusing on Targeted AI Applications:
Instead of aiming for general AI that can handle all aspects of healthcare, focus on developing specialized AI tools for specific, high-impact areas such as:- Radiology image analysis
- Medication management and drug interaction prediction
- Administrative task automation
- Population health management and risk stratification
- Investing in AI Education and Training:
- Develop AI literacy programs for healthcare staff at all levels
- Create interdisciplinary teams that combine clinical, technical, and ethical expertise
- Foster partnerships with academic institutions to stay abreast of the latest AI developments
- Embracing Incremental Progress:
- Set realistic expectations for AI capabilities and timelines
- Celebrate and learn from small wins in AI implementation
- Develop a long-term AI strategy that allows for gradual scaling and improvement
By adopting these strategies, healthcare organizations can continue to make meaningful progress in AI implementation, even if the pace of advancement is slower than initially anticipated. The key is to remain flexible, focus on areas where AI can have the most immediate impact, and continuously adapt our approach as the technology evolves.
A More Realistic Vision for 2030
While the potential of AI in healthcare remains enormous, it’s crucial to temper our expectations with realism. By 2030, we’re likely to see significant advancements in healthcare AI, but perhaps not the sci-fi vision of AI doctors replacing humans or solving all of healthcare’s challenges. Instead, we might expect:
- More accurate diagnostic tools and decision support systems
- Improved administrative efficiency through AI-driven process automation
- Better predictive models for population health management
- Advances in personalized medicine, though perhaps not at the individual level for all patients
As healthcare leaders, we must prepare for an AI-augmented future, but also recognize the limitations and challenges we face. Our focus should be on developing AI systems that complement human expertise, enhance efficiency, and improve patient outcomes within the constraints we’re likely to face. The journey towards AI-driven healthcare will be more of a marathon than a sprint. By acknowledging the potential roadblocks now, we can work towards overcoming them, ensuring that AI can deliver on its promises to improve healthcare, even if it doesn’t quite reach the “promised land” by 2030.



0 Comments