As we mark another Breast Cancer Awareness Month, it’s crucial to reflect on both the progress we’ve made and the challenges that lie ahead. Breast cancer remains the most common cancer among women in the United States, accounting for about 30% of all new female cancer cases each year. The American Cancer Society estimates that in 2024, we’ll see approximately 310,720 new cases of invasive breast cancer diagnosed in women, along with 56,500 new cases of ductal carcinoma in situ (DCIS). About 42,250 women will die from breast cancer. This is a stark reminder of the ongoing battle against this life-threatening disease, but thankfully we are also on the cusp of a transformative shift in how we approach breast cancer screening. Traditional methods—although effective for many—often suffer from limitations such as accessibility, convenience, and timeliness. However, exponential technologies are reshaping the landscape, making individualized breast cancer screening more accessible and personalized than ever before. The next frontier in breast cancer detection lies in empowering individuals through technology-enabled, self-directed screening—a shift that promises to save more lives and improve health outcomes.
The Current Challenges of Breast Cancer Screening
Early detection remains one of the most critical factors in improving breast cancer survival rates. Yet, many women still face significant barriers to regular screening. In low-resource settings or rural areas, access to mammography centers can be limited, and even in well-resourced countries, long waiting times or logistical challenges often delay life-saving diagnoses. While mammography remains a critical tool in breast cancer detection, it is not without drawbacks. Some of the key harms associated with traditional screening approaches include:
- Overdiagnosis and Overtreatment: Screening often detects cancers that may not be life-threatening, yet standard treatments such as surgery, radiation, chemotherapy, and hormone therapy are applied universally. It is estimated that 20-50% of screen-detected cancers represent overdiagnosis, leading to unnecessary treatments for many women.
- False Positives and Anxiety: Mammograms frequently result in false positives, leading to further testing and emotional stress. In the U.S., about 10% of women are recalled for additional testing, though only 0.5% are diagnosed with cancer. Over a decade of annual screenings, approximately 50% of women experience at least one false positive, and 7-17% undergo unnecessary biopsies.
- False Negatives: In some cases, mammograms fail to detect breast cancer, particularly in women with dense breast tissue or certain cancer types. False-negative rates range from 6% to 46%, potentially leading to delays in diagnosis and treatment.
- Radiation Exposure: While the radiation dose from a single mammogram is low, there is a theoretical risk of radiation-induced breast cancer with repeated screenings. Estimates suggest that for every 1,000 women screened annually from ages 40 to 80, up to one case of breast cancer may be caused by radiation exposure.
The standard “one-size-fits-all” approach to breast cancer screening also fails to account for individual risk factors, which range from genetic predisposition to lifestyle and environmental influences. Today, a growing body of evidence suggests that more personalized screening protocols—tailored to an individual’s risk profile—can dramatically improve early detection rates and reduce unnecessary interventions.
The Promise of Self-Administered Screening Technologies
The future of breast screening, as envisioned through Dr. Pillay’s lens of “prosumerization”, demands a shift where individuals are not just passive recipients of care but active participants, equipped with the tools to detect and manage their health. Self-administered screening technologies are emerging as a promising complement to traditional methods. These innovative approaches aim to empower individuals to take an active role in their breast health, potentially increasing screening rates and enabling earlier detection. Let’s explore some of the groundbreaking technologies in this space:
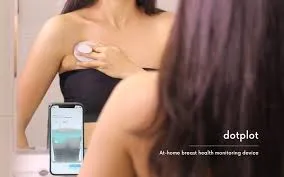
- DOTPLOT: This UK-based startup has developed a handheld device that uses sound waves and AI to detect abnormalities in breast tissue. Users can perform scans at home, with data analyzed through a smartphone app. DOTPLOT’s technology aims to provide a comfortable, radiation-free option for regular breast checks.
- MIT’s Ultrasound Technology: Researchers at MIT have created a low-cost, handheld ultrasound device that can be used for breast self-examinations. This technology uses machine learning to interpret the ultrasound images, potentially making breast cancer screening more accessible and affordable.

- Galleri Multi-Cancer Early Detection Test: While not specifically for breast cancer, this blood test developed by GRAIL can detect multiple types of cancer, including breast cancer, at early stages. It works by identifying DNA shed by cancer cells in the bloodstream, offering a non-invasive screening option.

- Smartphone-Based Solutions: Several apps and attachments are being developed to turn smartphones into breast cancer screening tools. For instance, the “Breast i” device, developed by a team in Ghana, attaches to a smartphone and uses light to detect angiogenesis, a hallmark of breast cancer.

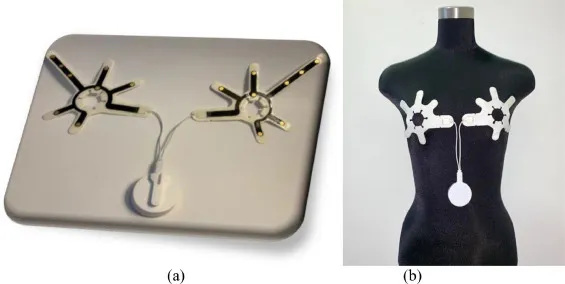
- Thermal Imaging Devices: Companies like Cyrcadia Health are developing wearable devices that use thermal sensing and AI to detect early signs of breast cancer. These devices monitor temperature changes in breast tissue, which can indicate abnormal cell growth.
While these technologies show immense promise, it’s important to note that they are at various stages of development and validation. Many are not yet FDA-approved for breast cancer screening and should be viewed as complementary to, rather than replacements for, established screening methods. As we move forward, rigorous clinical trials and regulatory approvals will be crucial to establish the efficacy and safety of these technologies.
However, the potential benefits are significant:
- Increased accessibility, particularly in underserved areas
- More frequent screening due to ease of use and reduced barriers
- Empowerment of individuals in managing their breast health
- Potential for earlier detection, leading to improved outcomes
Conclusion
The future of breast cancer screening is evolving rapidly, with self-administered technologies poised to play a significant role. As healthcare leaders, we must stay informed about these innovations and work towards their responsible implementation. By embracing these technologies, we have the potential to detect breast cancer earlier, save more lives, and ultimately, work towards a world where breast cancer is no longer a life-threatening disease.
This Breast Cancer Awareness Month, let’s celebrate the innovative spirit driving these advancements and renew our commitment to improving breast cancer detection and care for all.



0 Comments